Mother’s Natural Childbirth Dream Comes True with AHN Midwives at Jefferson Hospital

Two simple hopes. That’s all Sarah Easton had for her third childbirth experience.
“An unmedicated, vaginal birth was absolutely what I was hoping for,” she said. “And that I’d have a healthy pregnancy.”
But based on her two previous pregnancies – during which she had gestational diabetes and high blood pressure – Sarah expected she may not realize that natural childbirth dream.
“Since I had some prior health issues, I was anticipating having them with this pregnancy as well,” she said.
But Sarah and her husband, B.J., believed that she was in the best possible place – under the care of AHN Midwives at Allegheny Health Network’s (AHN) Jefferson Hospital in Pittsburgh’s South Hills. AHN Midwives, the region’s only hospital-based midwife program, had managed Sarah’s prior pregnancies.
“I got to know them well and got to be very comfortable with them,” said Sarah, who lives in Moon Township, nearly 30 miles from Jefferson Hospital. “After the birth of my second baby, we knew we’d make the drive to deliver with them again.”
Not only did Sarah take comfort in knowing AHN Midwives would do everything possible to help her have the natural, unmedicated childbirth she wanted. But also, she knew that if complications arose, she’d have direct access to women’s health doctors and the full resources of Jefferson Hospital.
That includes emergency care and a Level II neonatal intensive care unit (NICU).
And as her pregnancy advanced, Sarah and B.J. realized Jefferson Hospital was right where they needed to be.
A nervous beginning
All looked well in the early weeks of Sarah’s pregnancy in spring 2018. At around 12 weeks, though, she visited AHN Midwives for a routine check-up and got quite a scare.
Certified Nurse-Midwife Amanda Shafton couldn’t locate the baby’s heartbeat.

“I started having a lot of anxiety,” Sarah said. “With my first pregnancy, I had some bleeding at around six weeks. I went to the emergency room, and initially, doctors thought I had a miscarriage. Although everything was fine, that scare has really stayed with me.”
Shafton immediately ordered an ultrasound.
“Once they said a heartbeat was there and I could see the baby, that anxiety went away,” said Sarah, who didn’t want to know the baby’s sex until delivery.
Sarah felt reassurance but remained cautiously optimistic.
A familiar problem returns
At 28 weeks, Sarah visited AHN Midwives for a routine exam. She felt fine. But her bloodwork painted a different picture.
Once again, Sarah had gestational diabetes.
“Moms often don’t have any symptoms,” Shafton noted. “But it shows in their blood sugar levels.”
If such issues arise, AHN Midwives consults with Jefferson’s women’s health doctors – who see patients on the same floor of the hospital.
“We teamed up to care for Sarah with our maternal fetal medicine experts, who would help monitor her going forward,” Shafton said.

Doctors ordered a precautionary ultrasound. It showed that the baby – a healthy six pounds – looked fine.
“They had me checking my blood sugar every three hours,” Sarah said. “I was able to regulate it with my diet, and I really had to watch my carb intake.”
Sarah had cleared a major hurdle. But nothing had prepared her for what would happen next.
A frightening jolt
In July 2018, Sarah was traveling by car with her family. Enjoying a leisurely summer day, they eased to a stop at an intersection.
Within seconds, though, their car shot forward when a driver hit them from behind.
“We were all pretty banged up,” Sarah said. “We went to the ER to have everyone checked over. They did an ultrasound, and the baby was fine.”
Thankfully, so were her other family members, including Sarah’s daughters Ella, 3, and Everett, 2.
Sarah, however, saw a chiropractor three days a week to get relief from her pain and soreness, hoping brighter days were ahead.
Still more challenges
But not long after the car accident, roughly 30 weeks into her pregnancy, Sarah had another health issue.
A check-up at AHN Midwives showed she had high blood pressure. If not controlled, it could put her and her baby’s health at risk, possibly meaning an early delivery.
Shafton and doctors had Sarah monitor her blood pressure daily. They kept it in check until Sarah and her baby reached 39 weeks – nearly full-term.
“I didn’t have to take medication for the high blood pressure,” she said. “It was kind of sporadic.”
Then, on Oct. 30, 2018, Sarah came to AHN Midwives for a final check-up. Shafton ordered another ultrasound.
That test showed yet new causes for concern. Sarah’s baby had grown quite large – nine pounds, seven ounces – a common occurrence in expectant mothers with diabetes.
Not only was Sarah’s baby possibly too big to allow for vaginal birth. But also, the baby’s shoulders could potentially become stuck during delivery.
“The baby could become injured,” Shafton said. “And this condition – called shoulder dystocia – could become an emergency with serious consequences for both baby and mom.”
And now, Sarah’s blood pressure started creeping up again. Although she and her baby weren’t in imminent danger, Shafton and the doctors knew they had to intervene.
They believed that Sarah still could achieve a vaginal delivery if induced. But a c-section might be necessary.
“At this point, I was very tired, and I left it up to them,” Sarah said.
Shafton asked her to return to Jefferson Hospital the next morning for delivery. Sarah’s dream of a natural childbirth hung in the balance.
A team approach – and joy at last
Around 8 a.m. the next day – Halloween – Sarah and B.J. arrived at Jefferson. They settled into the hospital’s birthing center, and Sarah was given medication to induce labor.
“In birthing circles, as long as no pain medication is given and delivery is vaginal, it’s regarded as a natural birth,” Shafton said.
At about 3 p.m., Sarah’s baby moved toward the birth canal.
“The contractions were very intense. I was up and moving to try and stay comfortable,” Sarah said. “I was in a lot of pain, and I was so exhausted that I asked for medication so I could hopefully be able to lay down and rest.”
But just as a nurse walked in with the pain medication, Sarah felt the baby moving. “It turned out I didn’t need the medication after all,” she said. “It was time.”
To ease delivery, Shafton used something called the Gaskin Maneuver.
“The mother is on her hands and knees on the bed, and her pelvis is more open,” Shafton said. “We knew that position might allow more room for the baby’s shoulders to come out.”
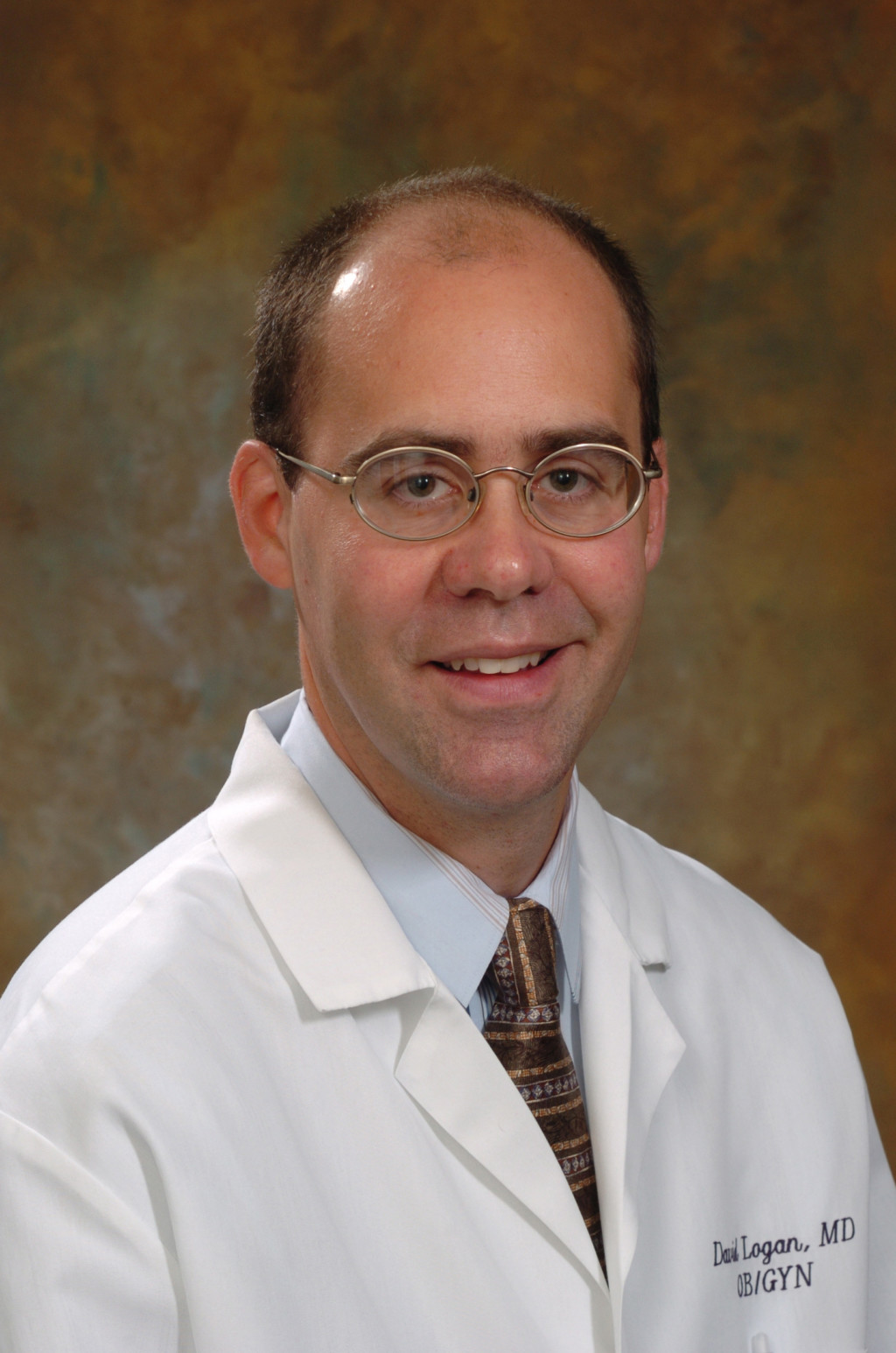
Typically, a nurse is the only one assisting a midwife during delivery. But in this instance, a care team surrounded Sarah: Dr. David A. Logan, chief of Jefferson’s department of obstetrics and gynecologic services; a neonatal certified registered nurse practitioner; and other nurses.
At 6:54 p.m., with minimal pushing, Sarah delivered a healthy baby girl – who she and B.J. named Emilia.

Finally – the testing, the worrying, and the waiting over – Sarah had realized her dream. And she and B.J. cradled their new daughter lovingly.
“We were overjoyed and just so thankful,” Sarah said. “Everything just went so beautifully.”
Mother and daughter stayed two days at Jefferson Hospital. On the day of discharge, the family had to overcome one last obstacle.
Emilia became ill suddenly. As a precaution, she was brought to Jefferson’s NICU, just down the hall from Sarah’s room, for observation. Two hours later, though, Emilia was cleared to go home.
Despite having to clear that final hurdle, Sarah and B.J. were thankful the NICU was so close.
“Everything at Jefferson, from the moment we walked through the door until the moment we left, was A-plus,” Sarah said. “I can’t say enough praising words. And I wouldn’t recommend anybody else but AHN Midwives.”